Loading...
Hospital billing
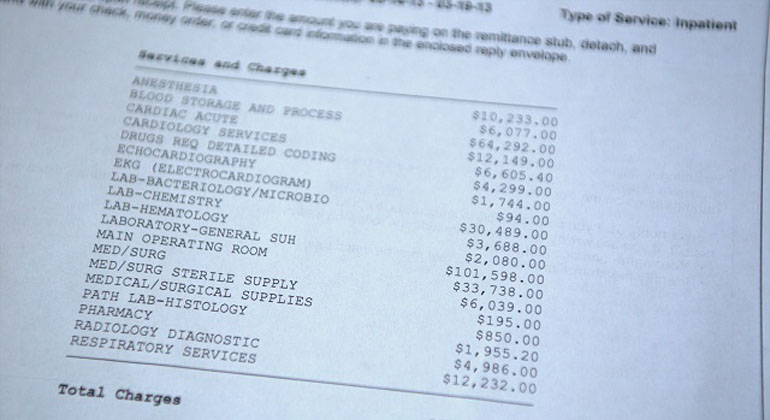
Hospital billing can be a very complex matter. It takes a lot of factors in consideration before being able to finalize a patient’s hospital charges. It might not entirely rely on the hospital or on the medical practitioner alone, but accurate hospital bill costing greatly depend on how the medical facility or doctor code diagnoses, treatment procedures, and other services provided to the patient.
To ensure a precise, easier, and faster computation and analysis of services or “products” provided by a hospital to a patient, a system has been developed that converts diagnoses and other health records to codes. Through such system, descriptive medical results and information are quantified, creating a constant calculation of a patient’s availed services. Some examples of medical coding include inpatient coding, outpatient coding, Emergency Department (ED) coding, and wound care coding
What factors can alter the hospital billing equation?
Hospital billing undergoes numerous procedures before being released, including the medical coding phase. Once all records are in code form, the coding manager will audit them and inspect for inconsistencies and/or anomalies during the validation, such as Discharged-Not-Final-Billed (DNFB) or Accounts Receivable (AR) charges.
What are DNFB and AR?
The cost of all services and products received by the patient in the hospital accumulate until his or her discharge date. Such expenses, however, when delayed for release beyond the patient’s discharge schedule will be called DNFB. The above circumstance often occurs due to several different reasons, including lack of medical coding adeptness. AR, on the other hand, is the account that has already been billed to a patient but is not yet paid.
How do hospitals regulate a patient’s hospital bill through the use of medical coding?
The Diagnosis-Related Group (DRG) is a system developed to scientifically classify medical cases to create a globally accepted hospital billing standard and equation. It negates the past cost-based matrix of hospitals which charge patients each service separately. DRG, charges the same cost to patients with the same conditions and services received instead, despite them undergoing different treatment and diagnosis routes.